35YR MALE WITH C/O ABDOMINAL SWELLING
This is an online E log book to discuss our patient's deidentified health data shared after taking his/her/guardian's signed in formed consent.Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence-based inputs .
A 35 year old male house contractor by occupation from Miryalaguda came to general medicine OPD with chief complaints of swelling in feet and abdomen since 2days
Tingling sensation,cough since 1 week , difficulty in intake of food.
History of presenting illness:
Patient was apparently asymptomatic 2days back then he developed edema in lower limbs which is insidious in onset gradual in progression and pitting type? and then he developed swelling in abdomen insidious onest gradual progression
h/o nausea ,tiredness and tingling sensation after eating food
No h/o vomiting, pain abdomen
H/o cough non productive type , because of cough he was having discomfort in food and water intake while swallowing.
Past history:
2 months back patient had distended abdomen feet swelling went to local hospital there he had tingling sensation and numbness hiccups also then they kept him in ICU for 3 days ,later he was referred to Kims
He was adviced for weekly checkup
N/K/C/O : Diabetesmellitus, Asthma , epilepsy, thyroid disorders, Hypertension
Personal history:
Patient now wakes up at 4 am , then
Have breakfast dosa , because of tingling sensation after food intake , he preferred not to eat anything
In evening he drinks jawa
Appetite is reduced
consumed mixed diet
Sleep disturbance since 2 years wakes up during sleep sometimes sleeps for 4 to 5 hrs and watches tv if he don't get sleep
Bowel and bladder movement are regular
Addiction for alcohol intake since 10 years intitially once a week and then it became 4 to 5 times a week of 1 quarter every time
(stopped from 2 months )
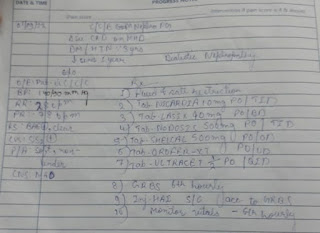
 Treatment history using lasix and lactulose syrup
Treatment history using lasix and lactulose syrup General Examination: Patient is conscious and coherent cooperative Vitals Temperature Pulse rate:Respiratory rate:GRBS:spo2Pallor-IcterusNo cyanosis,clubbing, edema -Head and neck - No alopecia Trunk- genecomastia present in right breastAbdominal distention present No loss of axillary hair ,No dilated veins
Palmar erythema -?
Systemic examination CVS - S1, S2 heard RS - BilateralAirEntry + , NVBS P/A -- SHAPE OF ABDOMEN - OBESE - ALL QUADRANTS MOVING EQUALLY WITH RESPIRATION.?NO SCARS AND SINUSES HERNIAL ORIFICES ARE FREE.- BOWEL SOUNDS +?CNSCRANIAL NERVES EXAMINATION - NORMALSENSORY SYSTEM- INTACTMOTOR SYSTEM EXAMINATON - NORMAL REFLEXES -
FINGER NOSE COORDINATION - PRESENTKNEE HEEL COORDINATION - PRESENT
PROVISIONAL DIAGNOSIS